Click title to see more…
The Sleep to Healthy website is now a 10 lesson course on curing insomnia.
This course is not a quick fix and it is not easy. The course is based on CBTi or Cognitive Behavioral Therapy for Insomnia. CBTi is the first-line insomnia treatment method endorsed by:
- The U.S. National Institute of Health and
- The British Association of Psycho-pharmacology.
- The American Academy of Sleep Medicine.
By the end of the “Cure Insomnia” course, students will have the knowledge and tools they need to cure their insomnia. Not just now, but for a lifetime.
Did I mention that it’s free?
Go to SleepToHealthy.com to get started.
Summary: Guest: Michael Swartz, creator of the Sleep on Cue App discusses:
- An example of someone who had multiple sleep disorders and how he dealt with it.
- Stimulus Control Therapy as part of Cognitive Behavioural Therapy for Insomnia (CBTi)
- Why you shouldn’t try to get to sleep.
- Intensive Sleep Retraining (ISR) as a way to get to sleep more quickly and sleep on demand.
- The Sleep on Cue smartphone app that mimics ISR and how it works
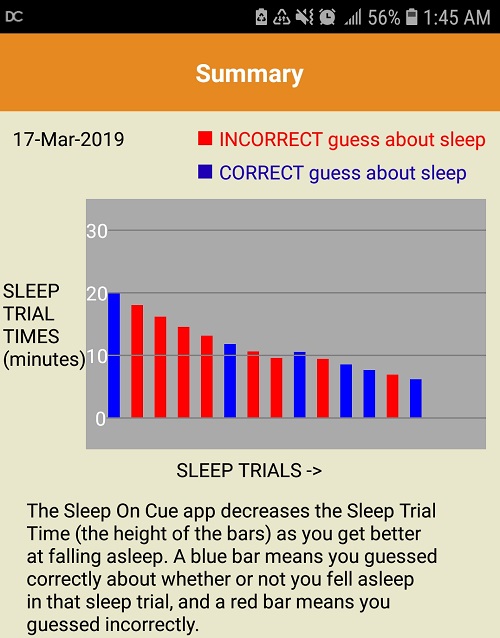
- Dennis talks about his experience with the Sleep on Cue app (his graph is at the bottom of the page)
- Why the Sleep on Cue app won’t work if you use it when you wake up in the middle of the night.
- Why you should include your regular doctor when trying to cure insomnia.
- Why you shouldn’t focus on getting 8 hours of sleep.
- Why reading before bed or when you wake through the night can be a good way to prepare for sleep.
Links mentioned in the show:
Michael Schwartz website: www.sleeponQ.com
Podcast: Sleep On It: http://www.sleeponq.com/sleep-on-it-podcast/
App: Sleep on Cue:
iPhone https://itunes.apple.com/us/app/sleep-on-cue/id829583727 ,
Android: https://play.google.com/store/apps/details?id=com.sleeponcue&hl=en
Twitter: @sleeponcue, https://twitter.com/SleepOnCue
Intensive Sleep Retraining (ISR): http://www.sleeponq.com/intensive-sleep-retraining/
Sleep Coaching: (Available via Skype): http://www.sleeponq.com/sleep-coaching/
Contact Michael Schwartz: http://www.sleeponq.com/contact-me/
Show notes with approximate time they occur in the episode:
(Note: For your convenience, the following is paraphrasing from the interview, not exact quotes. For exact wording, listen to that part of the episode)
Introduction:
We started today’s episode with some different music. It is a recording of today’s guest Michael Swartz. He opens his podcast episodes by playing blues on the harmonica, so I asked if he would provide some music for this episode and he assented.
Insomnia is complex, but 2 common issues are not being able to get to sleep at the start of the night termed “Sleep onset insomnia”, and waking up through the night and not being able to get back to sleep called “Sleep Maintenance Insomnia”. It can be frustrating laying in bed as the clock slowly ticks by, wanting desperately to fall asleep, but not having direct control over the elusive switch that puts our brain in sleep mode.
Maybe it’s even more frustrating for us since we live in a hyper-in-control society where our needs are tended to 24-7 giving us what we want, where we want and when we want it. And yet here is sleep, eluding our desperate pleas. Maybe sleep will come in now. Or now. Or now.
The time that elapses from when we lay down to when we get to sleep is called the sleep latency period. We can’t force sleep to happen, but we can find ways to help it perform its magic without such long, frustrating delays. And that is what we are going to talk about today – finding ways to get closer to our goal of sleep on demand.
We are fortunate to have as our guest Michael Schwartz, CEO of MicroSleep, LLC, an organization devoted to improving sleep health and wellness. Michael is the Program Director of the Clinical Sleep Health and Polysomnography Program at Oregon Tech University. Michael has over 30 years as a sleep professional.
Michael has his own podcast called “Sleep on It” and he developed a smartphone app called Sleep On Cue. I have listened to Michael’s episodes and bought and tried out his app and I was so impressed that I asked him to join us on our show. Michael, welcome to this episode of the Sleep to Healthy Podcast.
3:10 – Michael give us an example of someone you struggled with sleep but was able to work their way out of it. It was somebody with three or four different sleep disorders when they tested him. He had narcolepsy, sleep apnea, and periodic limb movement. It really impressed on him how complex sleep issues can be. They were able to help the patient understand what the issues were. It was complicated by him being a Greyhound bus driver. They started him on a CCAP for his sleep apnea and medications first for narcolepsy and cataplexy and the periodic leg movements resolved itself on its own. He learned that it’s not uncommon for more than one thing to be going on when they’re having trouble sleep with sleep. That was one of the more interesting cases that he dealt with.
5:50 Michael tells us about stimulus control therapy which is one of the main components of cognitive behavioral therapy for insomnia, CBTi. Our brain is associative, it is associates places and events with physiological states. It is almost continuously doing that. So it also helps in terms of sleep because the same happens with sleep. People with insomnia tend to spend a lot of time in bed awake while they are trying to get to sleep or get back to sleep. They do mental gymnastics to try to get their brain to go to sleep. But the brain has learned to associate the bed and bedtime with alertness and anxiety. Stimulus control therapy is an attempt to reverse this conditioning. The person is instructed to only be in bed if they are truly sleepy or they are asleep. This means they are removing themselves from bed if those two conditions are not being met. And the more they can do that the more chance there is that the conditioning can be reversed. It is true Pavlovian conditioning at work.
8:20 – Michael talks about how you can’t make or force yourself to sleep, you normally can’t sleep on demand. Sleep is a 100% passive event. Going from wakefulness to sleep involves an absence of effort. The only way sleep has a chance of happening is to completely avoid the effort to sleep. It is common in our language to say things like I’m going to try to go to sleep now. But that is misleading. He equates trying to focusing. Sleep needs mental focus to be somewhere else than on sleep. So he personifies sleep by saying things like “sleep needs you to do this” or, “sleep needs you to not do that”. It doesn’t guarantee sleep, but not focusing on sleep is a requirement for the onset of sleep.
10:40 – Michael explains intensive sleep retraining or ISR which is close to sleep on demand. It is a technique that was developed by some Australian sleep researchers how about 10 years ago. It is repeated short opportunities to fall asleep. In traditional stimulus control therapy, if sleep was not coming easy at the start of the night you would be instructed to get out of bed. And then go back to bed when you feel like you are truly sleepy again. Then later if sleep is a game elusive, to get out of bed again. Then go back to bed when you feel sleepy again. It is an effective strategy, but it can be a bit unstructured. So the Australian researchers decided to structure it by giving yourself a short time to see if sleep happens, and if it doesn’t we will instruct you to get her to bed and then shortly after that lay back down. It is preceded by intentional sleep deprivation. They did this intensive sleep retraining or ISR in a sleep laboratory with EEG (electroencephalogram) probes stuck to the patient’s head. The patients came into the laboratory around bedtime to start the process. The intensive sleep retraining or ISR works by having the patient sleep deprived at home by having more no more than 5 hours in bed the night before. So the homeostatic sleep drive was pretty strong, they were pretty sleepy. They were instructed to lay down and we’re given about 20 minutes to fall asleep. If the patient had not fallen asleep then the technician went in, knowing whether or not the patient had fallen asleep from the recordings on the EEG, and they would tap the person on the shoulder and ask them if they thought they had fallen asleep or not. The patient would answer, and then the technician, who knew the correct answer because of the EEG readings, would tell the patient if they were right or wrong. Correct or incorrect. If the person did fall asleep within the 20 minutes, the technician would let them sleep for a couple of minutes, and then went in and tapped him on the shoulder, knowing they were asleep at that point, woke the person up, asked them if they thought they had fell asleep, the person said yes or no, and the technician would give them the correct answer. Then, regardless of whether the person had fallen asleep or not, the person would be instructed to get out of bed. Then on the next half hour they were instructed to lay back down and repeat the whole process. Given a 20-minute opportunity to fall asleep, giving feedback, have to stay up until the next half hour mark. This was repeated 50 times which took 25 hours to complete the intensive sleep retraining or ISR. From bedtime to bedtime. So in a nutshell, that is intensive sleep retraining.
15:30 – Michael talks about the Sleep on Cue smart phone app for Android and iPhone that he developed that mimics this process intensive sleep retraining or ISR. He developed the app out of a call to action. In 2012 a study had shown that this type of training really helped with insomnia. It was compared with a group that did traditional stimulus control therapy for about 4 weeks. So they compared this 25 hour intensive sleep retraining or ISR program with a 4-week program. And they found that the results were essentially equivalent. They also followed up with the patients up to six months later, and they found that the improvements held. During intensive sleep retraining the person is sleep deprived more and more as the 25 hours progresses, so they were concerned that the learned ability to get to sleep more and more quickly was mainly driven by the greater and greater sleep deprivation. But what it proved was that the brain was actually learning to get to sleep more and more easily, at least partly due to the feedback given with each session. In essence they learned what being sleepy and falling asleep felt like. Dr. Spielman and Glovinsky, two very well-known sleep researchers who reviewed the study, which commented on this remarkable finding and how effective it was, and concluded the review by talking about how technique to do in intensive sleep retraining in a non laboratory setting – at home, needed to be created. He remembers in 2013 staring at that paragraph and thinking yes, this really needs to be developed. And that lead him on the journey to develop to sleep on cue phone app. He started out by trying to develop a handheld device with an accelerometer, battery, you hold in your hand and drop it when you fell asleep. With a smartphone was a natural fit for it because it has a built-in accelerometer.
19:40 – Michael explains how the app works. Ideally this is done after a poor night’s sleep the next night when you are already naturally tired. He tries to follow the original is our protocol. But he did not want people to intentionally be sleep deprived themselves as this was not a good idea for legal & safety reasons. So if you’ve had a poor night sleep on your own, which is usually not a problems for people who are interested in the app, then start to use the app the following night. So at bed time you start the app and you hold the phone in your hand. You let yourself drift off to sleep. After bit of time the phone will vibrate which alerts the user they need to wake and answer the question of whether or not they think they had fallen asleep. If they were just asleep, then it wakes the person up. You can’t get into a deep sleep in just a couple of minutes so it is never a problem with it not waking you up. You answer the question, yes you were asleep or no you’re not asleep, and the phone immediately gives you the correct answer. So you are told whether your perception of whether you were asleep or not was correct. Then the app asks if you want to do it again, if you want to do another sleep trial. If you answer yes, then it prompts you to get out of bed for a few minutes, it has a built-in countdown timer, and then the process repeats. During the sleep trial, the way the phone tells whether you have fallen asleep or not, is by emitting a faint audible tone that sounds similar to a faint foghorn. Instruction is that when you hear the phone, to give it a little shake or a little jiggle. That activates the accelerometer in the phone and so the app knows that you are still awake. If you are asleep you will not hear the tone. This method is based on some research done in the 1960s where they found that our sensitivity too noise falls drastically when we get into Stage 2 sleep. Stage 2 sleep is our most common sleep stage and starts a couple minutes after you fall asleep. So the app can tell right as you reach stage 2 sleep. In stage 1 sleep, which is the initial stage of sleep when you first just off to sleep, very often people did not think they are asleep. It is transitional sleep.
24:20 – Dennis talks about his experience with the Sleep On Cue app.
First, you have to have a lot of self-discipline, it is not fun waking up over and over and over again when you are already sleep deprived. So you have to be willing to suffer a bit in order to reap the benefits. The second thing is it takes a bit getting used to because it feels awkward to be holding your cell phone while you drift off to sleep but adapted to it pretty easily. The third is that although it’s a learning process it is not like learning other skills. It is very intuitive. You’re not following specific instructions. You just have to relax and trust it. The app produces a graph of the time it takes to fall asleep with each trial. Dennis will put his graph on the episode notes of one night’s trial of 14 trials. Dennis went from taking over 20 minutes to get to sleep down to 7 minutes. Part of it is due to be being more and more sleep deprived. He also noticed that after finally going to sleep after the 14th trial that his sleep was deeper and more restorative than he could ever remember.
27:00 – Michael responds to Dennis observations. The app is a sleep trainer, not a sleep tracker, so it does take work. A sleep tracker is passive, it might be worn on your wrist or you may put your phone underneath your pillow and it just tracks your sleep. His app is a trainer and is designed to reverse the classical conditioning which is preventing people from falling asleep. If you go to the gym to condition your muscles, it is very salient, you can feel the additional strength and see your muscles getting larger. With sleep it is more subtle. The app gives you unlimited number of Trials. The original experiment had 50 trials over 25 hours. The app allows you to have more trials per hour since the time is variable and not restricted to every 30 minutes as the original experiment was. Michael recommends doing 12 to 15 trials minimum. After you finish the trials, you just put the phone down and go to sleep. Like the gym, it may not feel very good while you’re doing the training, but you do it for the results that you desire. The same goes for this training app. Michael encourages people to self-regulate and decide how many trials they do, to stop when they really don’t feel like doing anymore, which usually means they are very very sleepy. The graphs are portable and can be emailed or saved. Michael encourages people to email him their graphs and he can comment on them. The graph shows two things, whether you’re falling asleep is getting easier, and whether you’re perception of whether you have fallen asleep or not is getting more accurate. The research indicates that it is this awareness of whether or not you had fallen asleep is actually what is reconditioning the brain. The height of the bar graph indicates the trial time, meaning how long it took to get to sleep. And the color indicates whether you guessed correctly how about being asleep or not. Red means that you’re mistaken, blue means that you are correct. So you want the bars on the graph to be getting shorter and Bluer.
35:30 – the app is not to be used in the middle of the night, just at initial sleep-onset when you are sleep deprived. The app is designed to minimize the impact of using a cell phone just before going to sleep. If you wake up in the middle of the night, follow traditional stimulus control therapy which is to get out of bed, do something boring until you are sleepy again, and then go back to bed.
38:40 – Tips and common mistakes for people who would like to give the app a try. The primary target for the app is for someone who has trouble falling asleep. People who wake up in the middle of the night and have trouble getting back to sleep would be a secondary target group. If a person is taking sleeping medication to get to sleep, and their doctors and they want to taper off from the medication, the app can be a good tool to help with that. One of the common goals when people are using CBTi is to have a later bedtime. The app can be used while you’re waiting for that bed time to arrive to practice going to sleep. It gives you a productive thing to do for your sleep while you’re waiting for your bedtime. It is meant to enhance CBTi, not replace it, as CBTi has several elements to it. It’s best uses for someone who is practicing CBTi and wants a quicker, more robust response to it.
44:00 – It took a lot of time and financial resources to develop the app, and that is why there is a small price for the app. Also, there are no ads, it is a one-time lifetime cost, it is not connected to Facebook or collecting of personal information, and it can run whether you are connected to the internet or not. Some people like to use your earbuds. It is important to use the volume controls to make the sound as quiet as possible. Like a distant foghorn. The app can also do structured naps.
47:10 – Michael shares sleep advice from his decades of experience. Occasional bouts of insomnia are perfectly normal. Sleep gimmicks do not work. He strongly encourages people to give CBTi a chance. It is a lot of work but well worth the effort. Let your regular doctor know about anything about your sleep if you’re struggling. There may be a associations between your medical condition and medications and sleep that you are not aware of. If you find that you get to sleep well but you are frequently waking up to the night, that could be an indication that there is a sleep disorder that needs attention and you should bring it up with your doctor.
51:30 – Michael’s 30 second YouTube video vision: Don’t buy into the message that you need 8 hours of sleep every night. We are all different, and there’s no good evidence that people in past generations slept no more than about six hours or so. So don’t pay heed to the message, and then get anxious about it, and turn to sleeping pills or alcohol as a solution.
52:00 – Something listeners can do today to sleep better tonight to feel and function better tomorrow. Go to Michael’s website sleeponq.com. He has a lot of resources available. A helpful behavior is to read with an incandescent light source next to you until you feel truly sleepy before you put yourself in bed. The same goes in the middle of the night if you have trouble getting back to sleep. It takes your mind somewhere, and removes the focus from sleep.


Sleep To Healthy Thoughts